
AI-Powered Claim Assessment For Health Insurance

Smarter. Faster. More Transparent Health Claims Processing
Xangam’s AI-driven platform transforms health claim assessments, bringing real-time fraud detection, medical intelligence, and regulatory-grade automation to both cashless and reimbursement claims.

A Modern Approach to Health Claim Investigations
Manual checks and outdated workflows slow down approvals, introduce errors, and allow fraud to slip through. Xangam solves this with a scalable, intelligent system built to monitor every step of the clinical and claim journey. From OCR to risk scoring- every claim is verified with clinical logic and behavioral data.
2000+ claims processed per hour
40–60% higher fraud detection accuracy
Full compliance with DPDP Act, IRDAI, and MeitY AI Governance
How It Works
Xangam’s health claim AI engine connects medical documents, diagnostic reports, and hospital patterns to identify red flags and accelerate low-risk claims. All in real-time.
Core Features
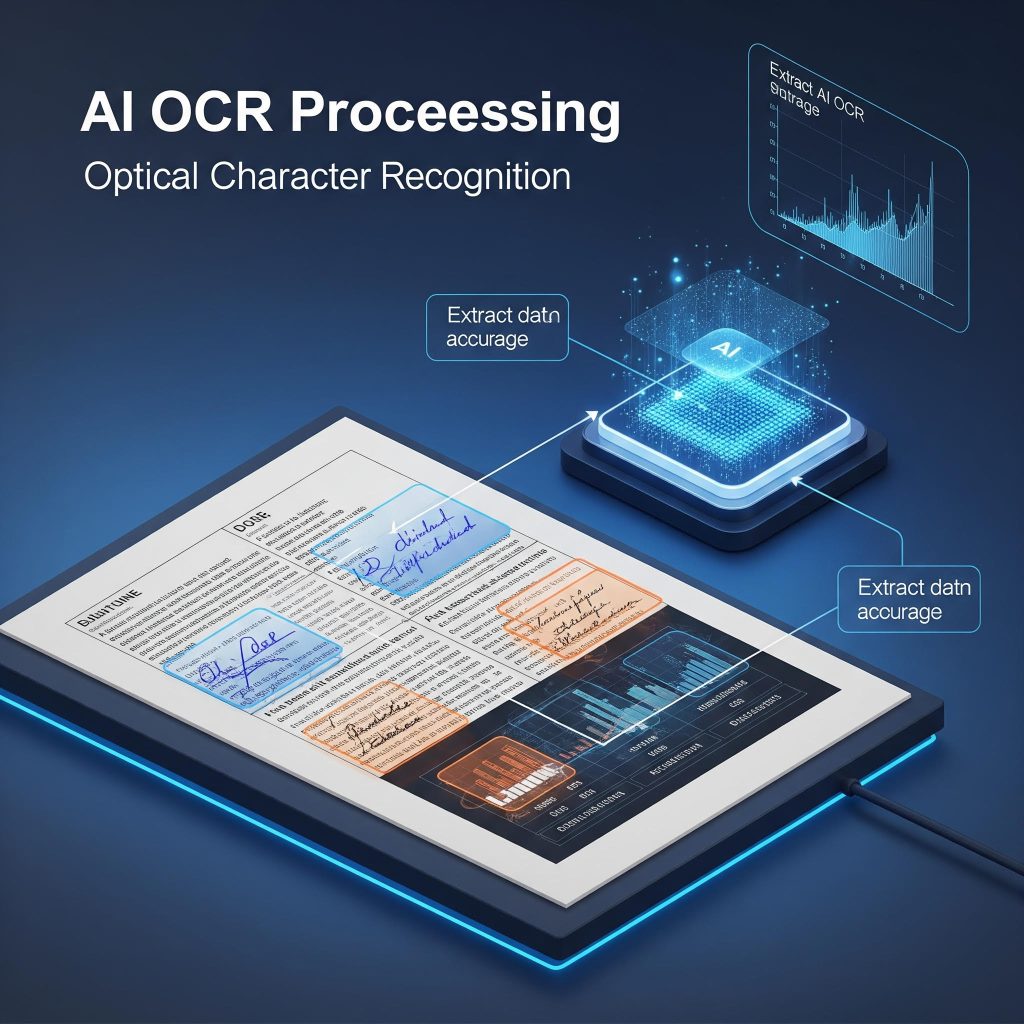
01. AI-Powered Document Processing (OCR)
Extracts critical data from discharge summaries, prescriptions, invoices, and lab reports with 95%+ accuracy, even handwritten text.
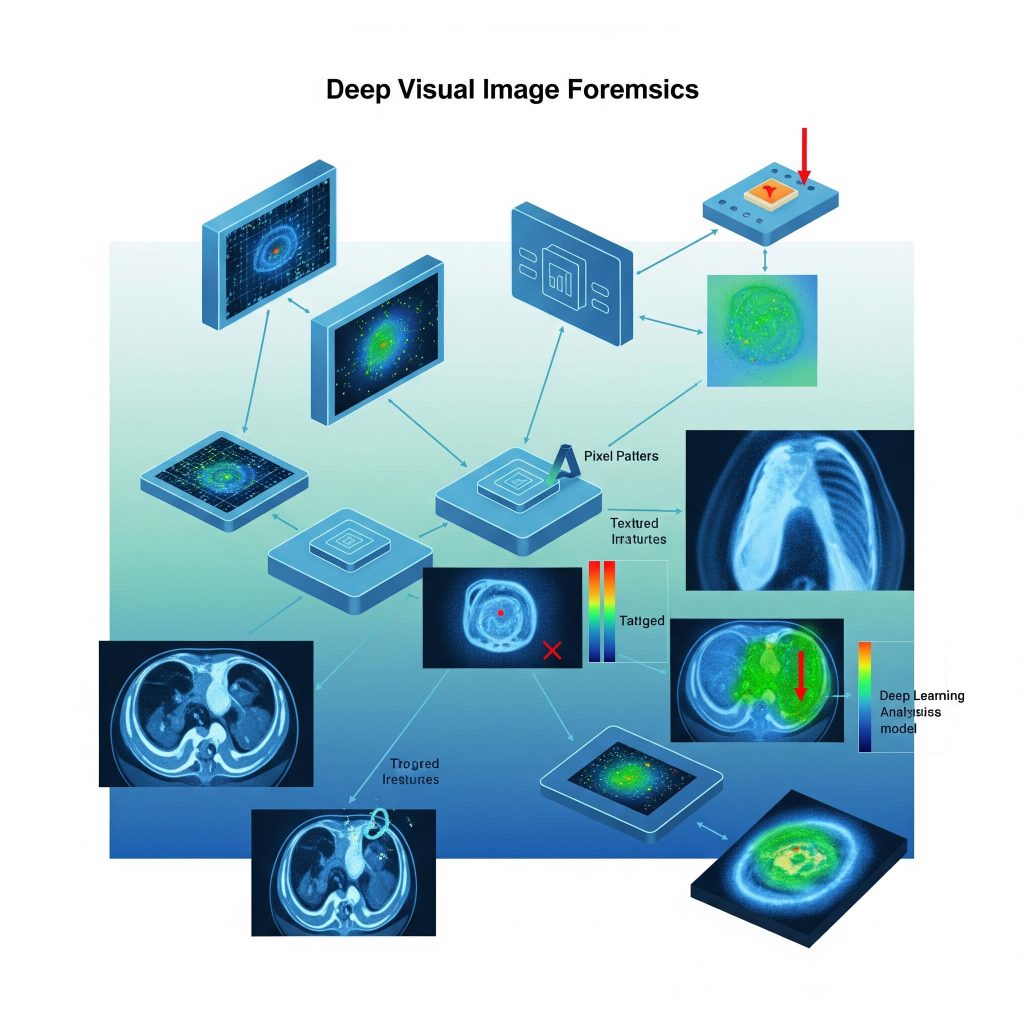
02. Medical Image Forensics
Detects tampered, forged, or duplicate diagnostic images using deep visual analysis and metadata inspection.
03. Automated Claim Classification
Auto-categorizes incoming claims by treatment type, hospitalization status, or policy conditions using machine learning classifiers.
04. Clinical Journey Mapping
Builds the patient's treatment timeline from unstructured medical records and compares it with standard clinical protocols.
05. Fraud Pattern Detection
Uses historical fraud data to detect red flags like inflated bills, duplicate treatments, or mismatched hospital-provider claims.
06. Real-Time Risk Scoring
Each claim is assigned a dynamic risk score across patient, provider, and claim levels to prioritize investigations instantly.
07. Explainable AI (XAI)
Provides clear, human-readable reasoning for every flagged anomaly or fraud prediction—ensuring auditability and regulatory trust.
08. Multilingual NLP for Health Claims
Understands and processes documents in 12+ Indian regional languages, removing translation dependency for TPAs and insurers.
09. Intelligent Entity Resolution
Connects disparate records like patient IDs, hospital codes, doctor names, and insurer systems to eliminate duplication and fraud.
10. Social Graph & Network Analysis
Uncovers fraud rings by mapping suspicious relationships between hospitals, doctors, patients, and claim histories.
11. Geo-Tagging & Timestamp Validation
Validates whether treatments happened where and when they were claimed using device-level metadata.
12. Medical Cost Benchmarking
Compares claimed treatment costs with market-standard pricing to detect overbilling or non-standard procedures.
13. TPA & NHCX Integration
Seamless integration with Third-Party Administrator systems and the National Health Claim Exchange (NHCX) via secure APIs.
14. Automated Pre-Check Rules Engine
Implements insurer-specific policies and IRDAI guidelines through a configurable rule engine for early-stage validation.
15. Adaptive Learning Models
AI models constantly improve based on new fraud trends, investigator feedback, and regulatory updates.
16. Real-Time Dashboards & Alerts
Live insights into fraud trends, investigation queues, and flagged anomalies, customized by role or region.
17. 100% MeitY & DPDP Compliant
Built to meet India’s AI governance laws, data residency mandates, and personal data protection regulations (DPDP Act 2023).


Why Choose us?
01. Purpose-Built for Health Insurance
Unlike generic AI platforms, our system is trained on millions of real-world health claims, designed specifically to detect medical fraud, abuse, and waste in Indian health insurance workflows.
02. Real-Time AI Risk Scoring
We don’t just detect fraud, we prioritize it. Our dynamic scoring engine flags high-risk claims instantly so your investigators can focus where it matters most.
03. End-to-End Automation with Human Oversight
From document ingestion to fraud alerts, the process is fully automated, but always explainable and auditable, with human control at every critical decision point.
04. Plug-and-Play Integration with TPAs and NHCX
Built for interoperability, our platform connects seamlessly with TPAs, core policy systems, and NHCX- no IT overhaul required.
05. Regulatory-First Design
Fully compliant with DPDP Act 2023, IRDAI norms, and MeitY AI Governance Framework 2025- so you stay future-proof and audit ready.
06. Proven Impact, Backed by Scale
Process over 2000+ claims/hour, reduce manual workload by 70%, and increase fraud detection accuracy by up to 60%; with clients seeing ROI within the first year.
Find Out How You Can Incorporate AI-Based Claim Assessment App for Health Insurance
Get your project kick started by filling details below